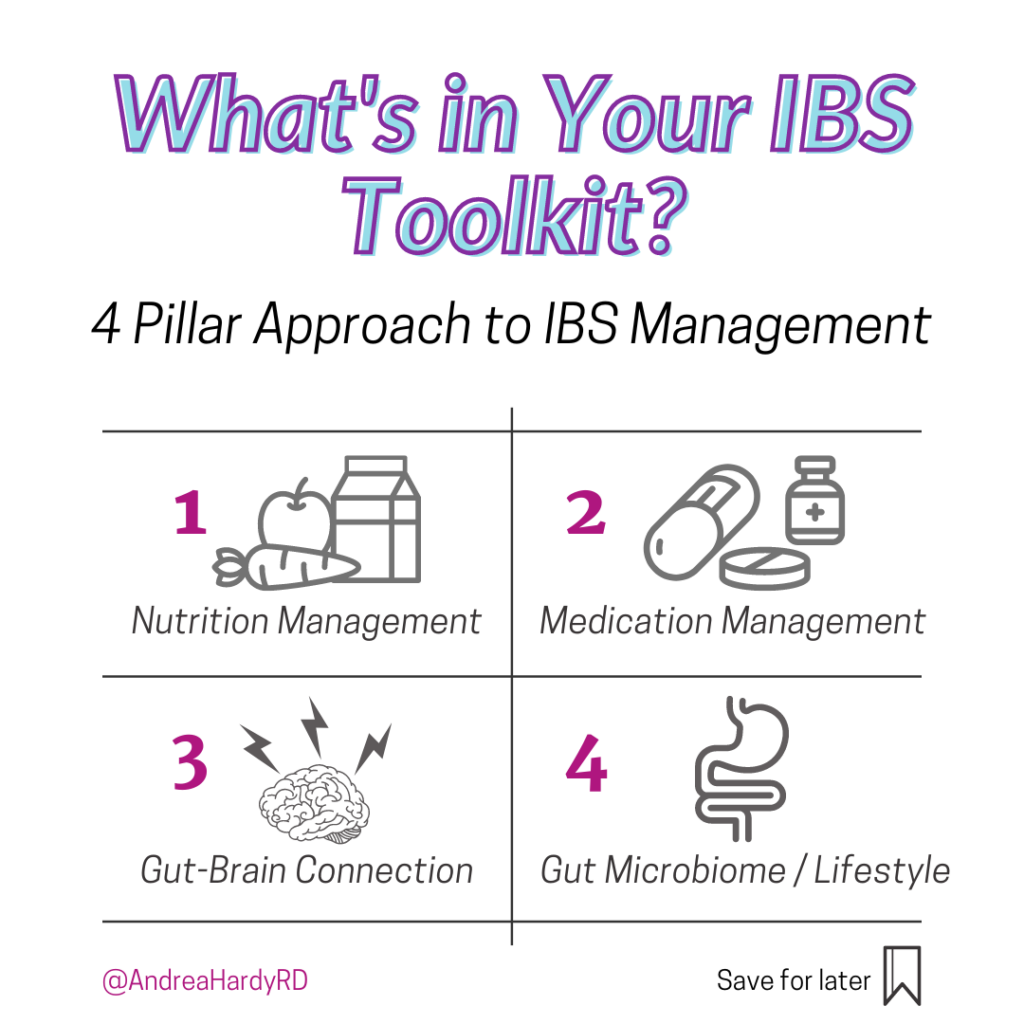
What’s in YOUR IBS toolkit? 🔨🔧💡🧰
Many times I see people JUST focus on nutrition. And with that – their lens for disease management gets REALLY teensy tiny.
While there’s a LOT we are still learning about IBS, what is incredible is the amount of research in different areas exploring tools for management!
@Ignite.nutrition.inc – we’ve come up with what we call our ‘4 Pillar Approach’. This encompasses a good chunk (although not all!) of the tools out there to manage IBS.
It includes:
- Nutrition management (the low FODMAP diet & other strategies)
- Medication management (both pharmacological and not)
- The gut-brain connection (stress management)
- The gut microbiome (we lump lifestyle into this pillar because it fits nicely with what we know about digestive health!)
Important of treating IBS outside of diet
As a dietitian, I work with patients on the nutrition component mostly – however I think it’s SO important to know about the other pillars so I can advocate for my patients and connect them to team members important in managing their care. I always say, I get WAY more time with the patient than many times the doctor does, and with a food first approach, I can get a good sense of when other strategies might need to be layered on to get symptom relief, or even when nutrition isn’t the most appropriate pillar to start with!
At the end of the day, there are SO many different strategies for managing IBS – not JUST nutrition – it’s all about finding the right one that works for you.
Is there a pillar you haven’t explored in your IBS management?
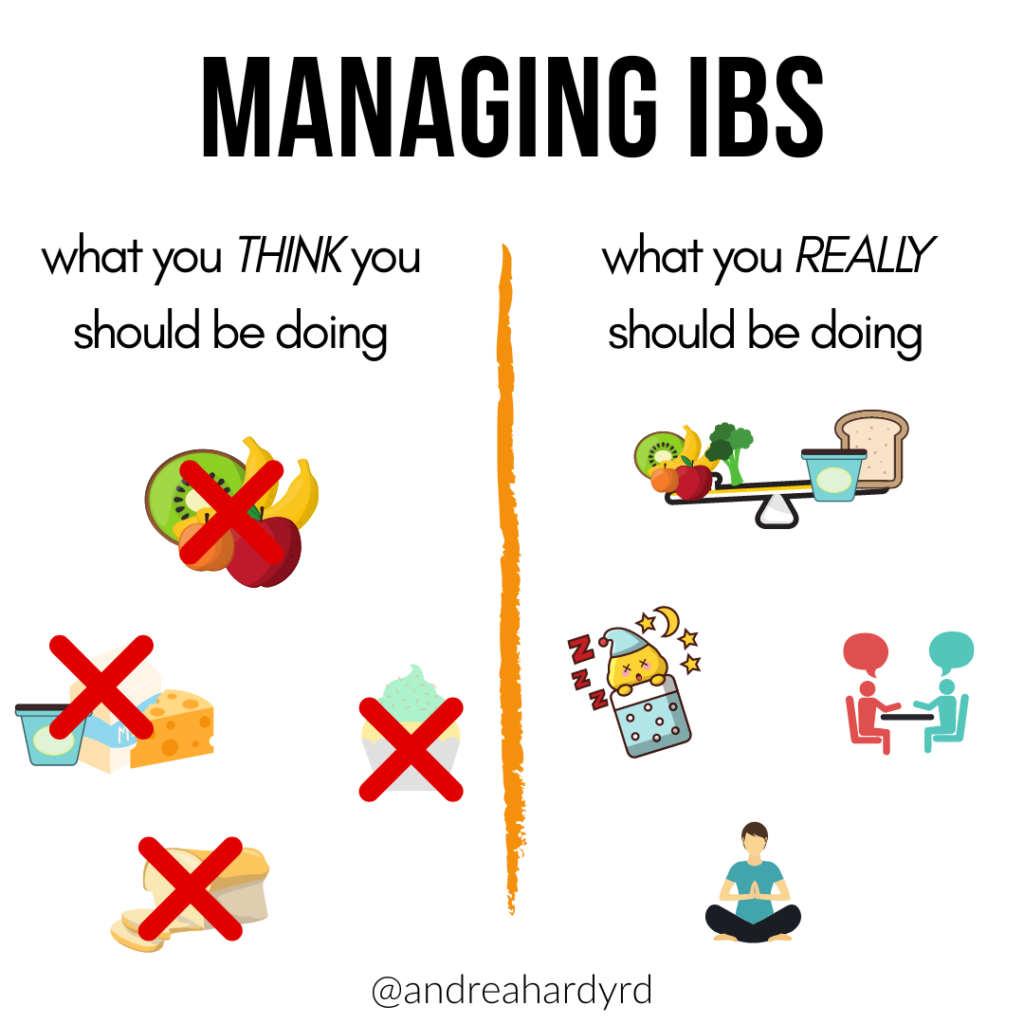
What you Should Really be Doing to Manage your IBS
🙋🏼♀️Who here agrees? 🙋🏼♀️
❌ I see far too many patients look to cutting foods out as their only IBS management strategy. The result? A short list of foods they feel safe eating, but often times – their symptoms aren’t THAT.MUCH.BETTER. ❌
Can I use the low FODMAP diet to manage my IBS?
✅While the low FODMAP diet can be considered an elimination diet – what we REALLY should be focusing on is what we can add in and how we can find balance.✅
⚖️The low FODMAP diet isn’t all or nothing, instead – I like patients to think of it as a ‘swap this for that’ – a way to figure out your triggers and in the end, liberalizing your diet to the fullest extent possible. ⚖️
In addition, FOOD isn’t the be-all and end-all of IBS management! In fact, many other lifestyle interventions perform just as well. 😴🧘🏼♀️🏃🏼♀️
What is the 4 Pillar Plan for IBS management?
@Ignite.nutrition.inc – we’ve developed our ‘4 Pillar Plan’ – that encompasses nutrition, stress management, medication management, and the gut microbiome.
The focus is on finding solutions that work for you that actually fit within your life, and understanding how your IBS is triggered. This can include things like working on sleep, stress, changes in exercise, focusing on ADDING IN low FODMAP items instead of focusing on ‘taking away’, and finding some good non-pharmacological and pharmacological strategies as needed to provide support.
To learn more about our ‘4 Pillar Plan’ – link in bio @andreahardyrd!
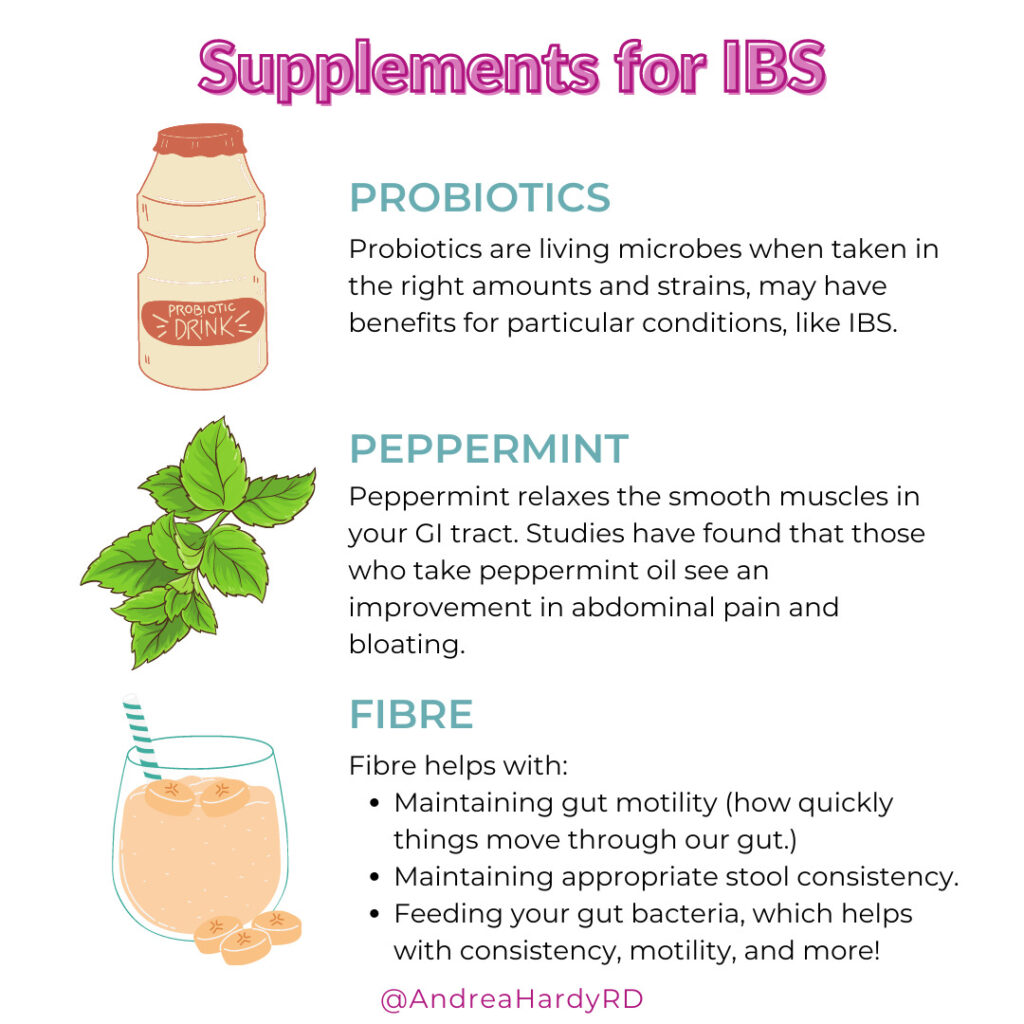
Supplements for IBS
Us dietitians are pretty wary of recommending supplements for our patients, but sometimes they are warranted or at least worth exploring. 🧐
In my practice, these are the top 3 supplement options I explore with clients to help alleviate IBS discomfort.
1️⃣ Probiotics.
These are living bacteria when taken in the right amounts and strains, may have benefits for particular conditions, like IBS. They should be taken for a period of time when you are not exploring other management strategies, so you can see how well they work for you.
2️⃣ Peppermint.
Yes, peppermint relaxes the smooth muscles in your GI tract. Studies have found that those who take peppermint oil see an improvement in abdominal pain and bloating. Some people like to drink peppermint tea, although the dose may not be the same. Another option is enteric-coated peppermint capsules. This means the oil is protected inside the capsule until it reaches the small intestine, where it can relax the lower GI tract.
3️⃣ Fibre.
In addition to feeding your gut bacteria, fibre helps with consistency, motility, and more! But it’s important to get enough: 25g/day for women, and 38g/day for men. If you are not able to get adequate fibre through food, you may benefit from a supplement.
⭐Some fibre options available in Canada are:
- Psyllium: Studies show this type of fibre provides symptom relief in both constipation and diarrhea predominant subtypes of IBS. It is often very well tolerated in IBS.
- Partially hydrolyzed guar gum: This type of fibre supplement is low FODMAP and has shown symptom relief in IBS patients – it is very slowly fermentable and seems to work very well in our IBS-D patients specifically.
- Methylcellulose: This type of fibre is non-fermentable, therefore does not generally have side effects such as gas production, bloating, or pain. It may be especially useful for those with IBS-C as it helps to soften stool with its gel-forming properties.
⚠️Caution
Inulin/chicory is a type of fibre that is high in fructans and therefore could potentially lead to more gas, bloating, and abdominal pain in those with IBS, and is a high FODMAP ingredient.
Don’t forget to download my free IBS guide! Link in bio.
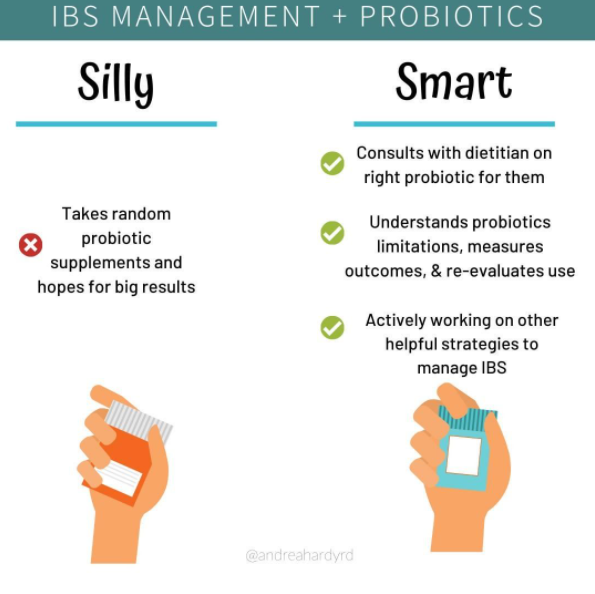
How to Manage IBS with Probiotics
❌. Most people don’t use probiotics properly.
In fact, I was prescribed antibiotics last week, and was told to take any probiotic or eat more yogurt with them.
I’m on the @AEProbio (the alliance for education on probiotics) scientific working group and am SUPER passionate about the proper use of probiotics!
I spend a lot of time educating dietitians, doctors, nurses, and pharmacists on the proper use of probiotics. What do I mean when I say ‘proper’?
You want to match the:
- The right strain
- To the right person
- For the right reason
In fact, Dragana, the clinical lead and creator of the Probiotic Chart sums it up perfectly.
Saying take a ‘probiotic’ is like telling someone to take ‘a drug’ for a urinary tract infection. Not helpful because you want to know what drug, in what amount, and for how long right?
SAME THING goes for probiotics! The strains are SO individual, and each strain has different evidence for different conditions. So – we want to ensure you’re taking the right strain.
I always explain to my IBS patients that probiotics add ‘marginal gains’. Probiotics may add symptom benefit but may not be the ‘be all and end all’ of your IBS management plan.
I like to add probiotics judiciously, when:
- Nutrition intervention isn’t the best option
- When nutrition intervention was inadequate
We trial them for 1 month, and then assess – are things better, worse or the same? And then re-evaluate.
So next time you choose a probiotic, make sure your provider reviews with you the strain, the dose, the length of taking that probiotic, and benefits for the condition you’re trying to treat!
Looking for help with your nutrition? Book an appointment with our private practice gastroenterology dietitians at Ignite Nutrition.
What should I do to manage my IBS?
Why is IBS management so expensive?
IBS management can be expensive – who agrees? 🙋🏼♀️
Well…. it can be, if you don’t have a plan in place. SO many tests & supplements exist that AREN’T evidence based❌
What does this mean? You’re wasting your 💰❗
🧪IgG testing – IgG testing does NOT have good quality evidence to support its use.
Yes. I know. There’s 1 slightly positive RCT. BUT.
The study design? Poor. Wheat & dairy, known FODMAP’s were primarily excluded in the true diet group not the sham group – so why do we need an expensive test for that when we have a highly evidence based approach to managing IBS that reduces intake of these foods?!
I hear ‘but some people feel better’ [point above] and ‘it helps improve patient compliance’ [Uhhh you charge $500 to ‘help patient compliance? Please explain the ethics of that.]
Bad IBS Management Strategies
- 🥚Glutamine. In 1 small scale human trial – beneficial to IBS symptoms and ?intestinal permeability. HOWEVER. We need to ask ourselves the population we’re using it in – the research is specifically in post infectious IBS-D. In our practice, it’s something we may consider if we’ve exhausted all other options because glutamine has low risk, and a small possibility of benefit.
- 💩Gut Microbiota testing. I’m so EXCITED for research to evolve – but fact of the matter is – the research is no where close using gut microbiota testing to dictate what diet we should follow. Go watch my IG TV video on this.
- 💊OTC General Digestive Enzymes. Great evidence for lactase, and alpha-galactosidase. Not great evidence for ‘general digestive enzymes’. Unless your pancreas isn’t functioning properly, you don’t need em.
What is worth it for IBS management
- 🥝Dietary intervention with a dietitian. This may be the low FODMAP diet, or a version of the NICE diet (or a combo of both!)
- 🏃♀️Exercise – Exercise has a CLEAR impact on IBS management. Not only is it good for IBS, but sleep, stress, and mood! Get some gentle movement into your day
- 💬Psychology – The gut brain connection OFTEN plays a role in IBS. Work with a psychologist to learn how tapping into your body awareness can transform your IBS symptoms.


Recent Comments