Have you heard of histamine intolerance? 🤔
Typically when you think of histamine, you think of allergies 🤧. But, histamine is also something we can ingest from foods and release from eating certain foods. Some people struggle with symptoms related to high histamine foods – this is called histamine intolerance.
Histamine is an important chemical messenger involved in:
- digestion
- brain function
- inflammatory response
- immune function
- and so much more!
Histamine is involved in our immune response to help increase blood flow to the affected area. Then, histamine is degraded and everything returns to normal. But what if we don’t break down the histamine after it continues to build up in the body?
This is where experts believe histamine intolerance stems from. It is a condition where a person is unable to adequately metabolize histamine, particularly histamine that they ingest from food. The primary theory is that those with histamine intolerance have a deficiency or impaired function of DAO and therefore experience allergy-type symptoms more often.
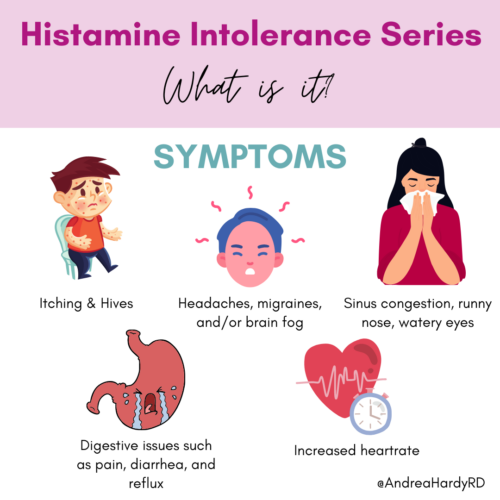
What are some of the common symptoms of histamine intolerance? 🧐
- Itching & hives
- Tissue swelling
- Low blood pressure
- Increased heart rate
- Throat tightening
- Anxiety or panic attacks
- Chest pain
- Sinus congestion, runny nose, watery eyes
- Headaches/migraines
- Fatigue, brain fog, confusion
- Digestive symptoms – abdominal pain, bloating, reflux, diarrhea
Histamine Intolerance Diagnosis
There is no currently clinically validated method to diagnose histamine intolerance. However, if a patient has more than 2 of these symptoms, and other conditions are ruled out, histamine intolerance may be worth considering.
How to diagnose histamine intolerance?
Histamine intolerance is difficult to formally diagnose! Why? 🤯
1️⃣ We have yet to determine a reliable biomarker to diagnose. (Serum DAO is suggested as a complementary test alongside other criteria though more research is needed to validate this).
2️⃣ Because the symptoms are SO non-specific and similar to MANY other conditions. They include: allergies, IBS, celiac disease, the list goes on! 🙄
Because of this, symptoms and response to therapy often guide the diagnosis.
That being said, it’s important we don’t jump to histamine intolerance based on symptoms alone. It is SO important that your health care team rule out other things first. Like IgE food or environmental allergies, or digestive disorders like celiac disease.
Once that is completed, your allergist might suggest an empiric approach (meaning, trial treatment and see if there is response)
Treatment Options for Histamine Intolerance
- Dietary intervention
- Considering using anti-histamines or DAO enzymes to assess whether an improvement occurs.
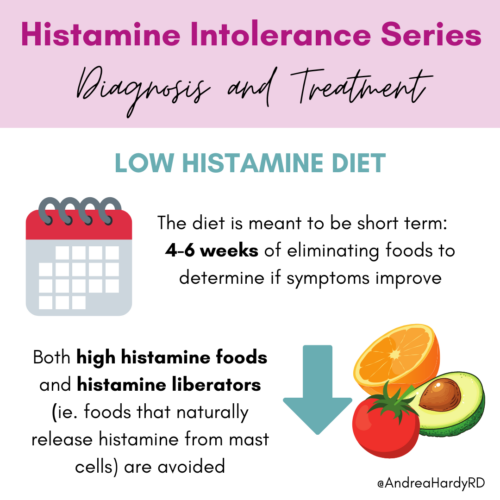
What exactly is a low histamine diet?
- Histamine is produced when foods have the chance to develop more bacteria. Like fermented foods, alcohol, aged foods, and foods that are not as fresh (ie. leftovers) are likely to cause more symptoms 🍷🧀🥓🍤🍳
- Some foods are histamine liberators. Meaning they trigger release of histamine from mast cells, but don’t actually have a lot of histamine themselves 🥑🫒🥫🍓🍋
- A strict low histamine diet should be short term ⏱ to determine symptom response and baseline, but it is important to work on liberalizing your diet to determine your threshold for histamine foods after that.
- It is highly recommended to work with a dietitian on following a low histamine diet. It can be restrictive and difficult to get all the nutrients you need!
Histamine Intolerance Medication
A low histamine diet one part of managing histamine intolerance. 💁🏼
However, medication is also a cornerstone in management too!
Other things that can impact histamine include:
- Alcohol
- Stress
- High intensity exercise
- Hormones like estrogen during menstruation
- Seasonal allergies
- Other environmental allergens like fragrance, mold, or pet hair
🪣 If we think of this like a bucket, there is only so much room for histamine. But, histamine can build up from several different sources. Therefore, a low histamine diet isn’t always “enough” to fully manage increased histamine in the body.
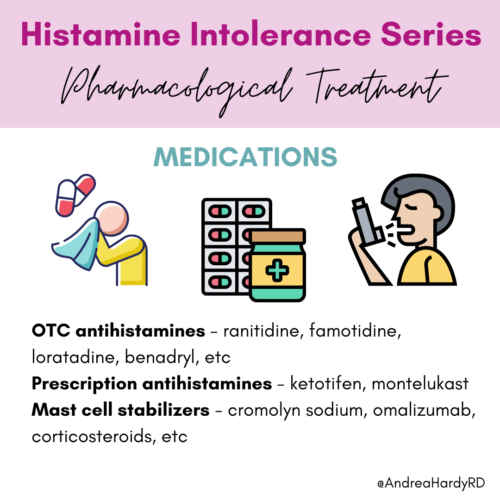
Antihistamines for Histamine Intolerance
💊 Despite minimal evidence at this point, experts/allergists often prescribe OTC antihistamine medications or H2 blockers helpful for symptom relief (empiric treatment). If inadequate, stronger prescription antihistamines or mast cell stabilizers are considered. However, there is one downfall to antihistamine meds – they only block histamine and don’t actually break it down after consuming histamine from food.
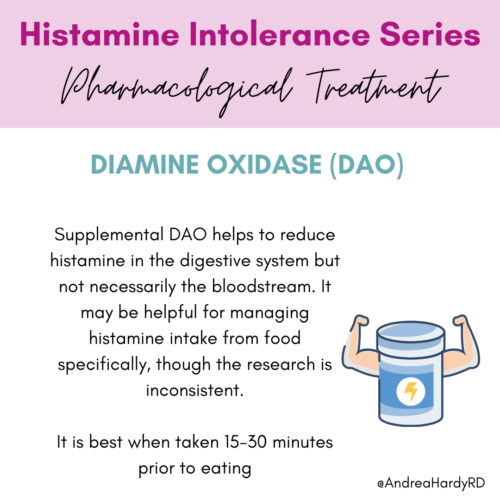
⁉️ Does such a product exist? Yes, BUT (there’s a but there). Since the main issue with histamine intolerance is believed to be due to a shortage or dysfunction in DAO (the enzyme that breaks down histamine), there are now DAO enzyme supplements on the market. While people often try DAO supplements to help degrade histamine and reduce symptoms, the research is rather iffy. Clinically speaking, I find them very hit and miss. So, in this way I don’t feel theory often lines up with use of these.
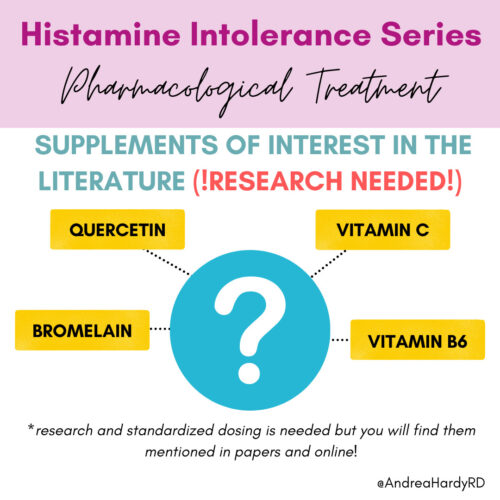
What about supplements for histamine intolerance?
🌿 ‘Supplements of interest but research is needed’ – I bring this up because I get asked by patients. Researchers are interested in how dietary supplements may help with breaking down histamine or stabilizing mast cells. In order to prevent release of histamine with things like vitamin B6, vitamin C, quercetin, and bromelain. But, we don’t have clinical trials yet. While these are often safe supplements, we don’t have data on this. So, always check with your doctor before trying these things for improving histamine intolerance.


Recent Comments