Did you know that there are 4 different proposed types of IBS? Let’s talk all about what you need to know about the 4 different types of IBS, the cause of IBS and the symptoms of IBS!
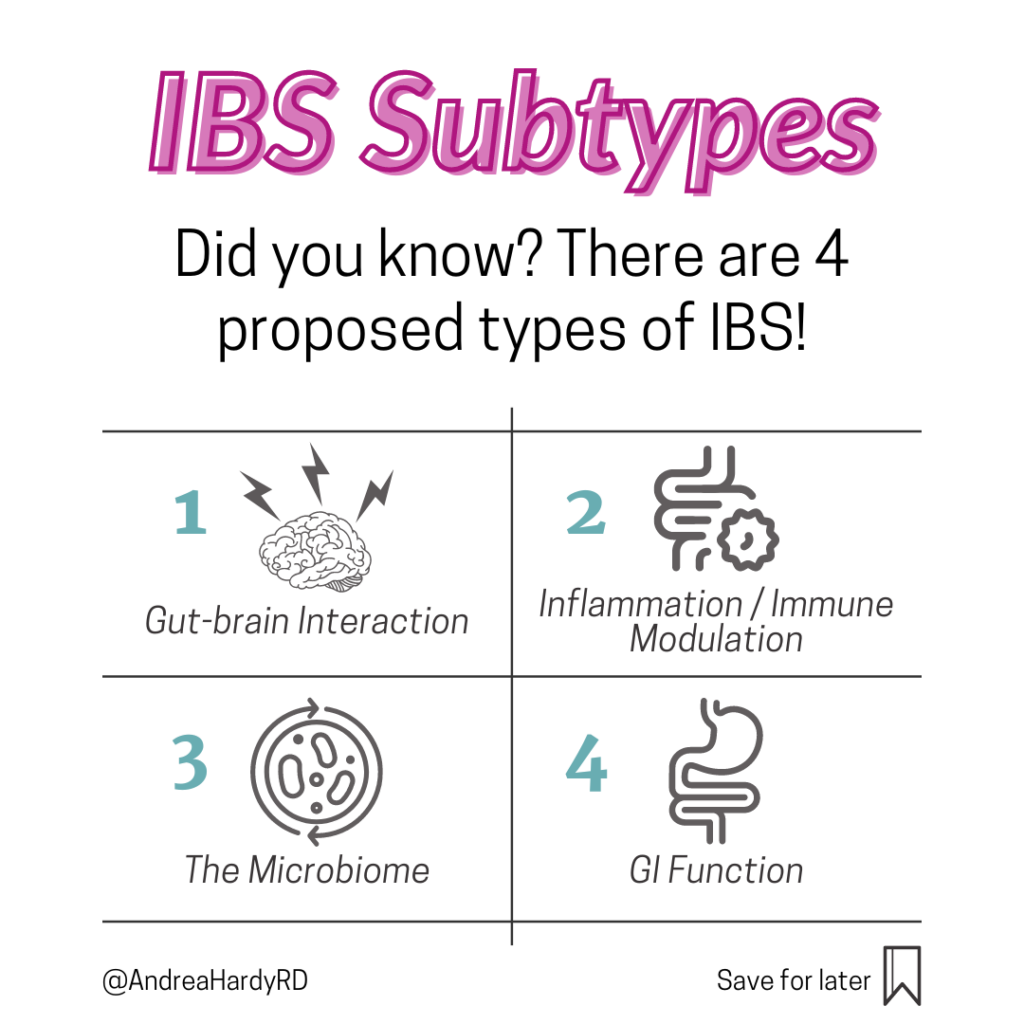
What types of IBS are there?
Is IBS 1 diagnosis? Or an umbrella diagnosis for many? ☂️
We’ve always known IBS is very heterogenous – meaning, not all cases appear the same, or respond the same treatment.
As research progresses, we’re beginning to be able to categorize IBS subtypes to better match the right person to the right treatment.
In fact, in an excellent review article published in 2020 by Nicolas Talley, he proposes pathophysiology based sub-typing to lead to better, more targeted interventions.
These include:
- gut-brain interaction
- inflammation/immune modulation
- the microbiome
- GI function
What’s important to note, is many times we don’t have diagnostic tools to ‘sub-type’ patients. In addition – you may fall into more than one sub-type!
This week on #LetsGutReal podcast, I interview Dr. Doug Drossman from @romefoundation on disorders of the gut-brain axis, and how our understanding of these disorders has changed over the years!
In the podcast, Dr. Drossman and I talk about how the gut-brain interaction plays a role in IBS, and what sorts of treatments exist to support that. It’s a MUST LISTEN. (I’ll say, I’m STILL star struck Dr. D let me interview him for the podcast).
In future posts I will tackle explaining the proposed mechanisms behind each one (though – let me tell you – many episodes of Let’s Gut Real do this already, so if you want to get a jump-start, start there!)
Oh and if you haven’t already, whether you’re a health care provider or patient – you HAVE to pick up your copy of Dr. Drossman and Johannah Ruddy’s new book ‘Gut Feelings – Disorders of the Gut-Brain Interaction and the Patient Doctor Relationship’ at http://drossmancare.com or Amazon!
DOI: 10.14309/ajg.0000000000000485
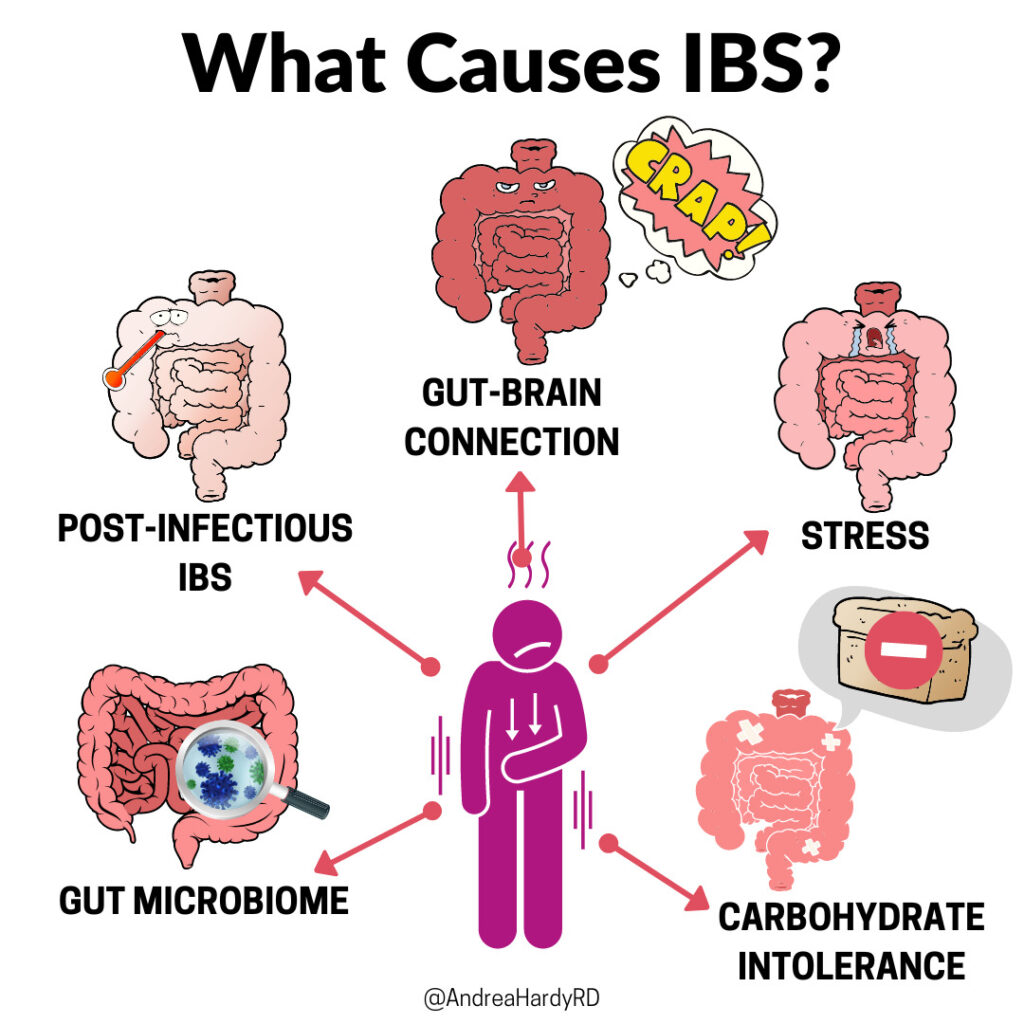
What Causes IBS?
IBS is a disorder of the gut brain interaction – while there is nothing structurally wrong with the gut, I think all of us with IBS can agree – it sure feels like it!
We don’t know the exact cause of IBS – however, research has implicated several possible causes, and it’s likely they all contribute in their own way!
A few potential causes of IBS include:
- 🤮Post infectious IBS – infection appears to modify the gut microbiota, intestinal permeability, and immune activation, leading to IBS symptoms
- 🦠 The gut microbiome – changes in the gut microbiome (possibly from food, stress, environmental exposures etc) can alter motility, sensation, gut-brain connection, immune activation and intestinal permeability.
- 😰Stress – alters the gut-brain interaction, changing digestion and increasing visceral hypersensitivity. When stressed we are often more sensitive to changes in our gut as well which can add more stress! Stress also appears to drive changes in the gut microbiome, immune system, and intestinal permeability.
- 🍞Carbohydrate intolerances – inability or reduced ability to digest certain carbohydrates, or increased sensitivity to the effects they exert of the gut (stretching by way of gas production and osmotic pressure triggers IBS like symptoms by way of the gut-brain axis). Newer research is exploring how carbohydrate fermentation may impact the gut microbiome, intestinal permeability & immune response (though the results are preliminary, in animals, and at very high doses – so no conclusions can be drawn yet).
As you can see, our gut-brain axis, immune system, and gut microbiome are central to all of these potential drivers.
It’s likely not just ONE cause but a disruption in many of these that leads to IBS!
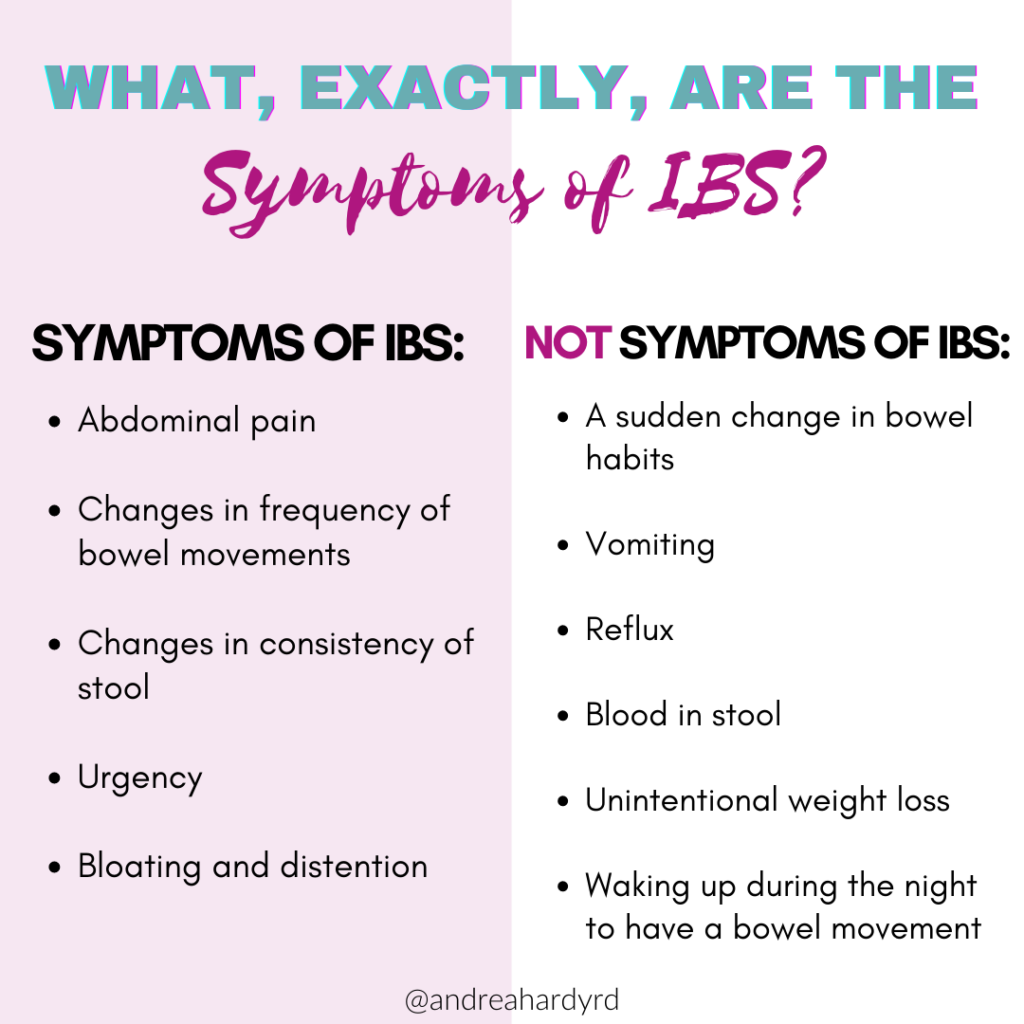
What are the symptoms of IBS?
Are your symptoms IBS, or could they be something else? 🚩
While IBS is common, it’s important to recognize, it’s not the ONLY cause of digestive symptoms, and even if you have an IBS diagnosis, if things change suddenly, they need to be re-evaluated!
Getting the right diagnosis is key – so what should you be watching out for?
✔️ Symptoms of IBS:
- Abdominal pain
- Changes in frequency of bowel movements (over >3 months)
- Changes in consistency of stool (>3 months)
- Urgency
- Bloating and distention
⛔ Not symptoms of IBS:
- A sudden change in bowel habits
- Vomiting
- Reflux
- Blood in stool
- Unintentional weight loss
- Waking up during the night to have a bowel movement
Is unintended weight loss a sign of IBS?
I had a patient who had been trying to lose weight, and despite not changing his approach, started to lose weight. He said his diet was ‘finally working’ but was a bit concerned because the weight loss was unintentional. In addition, his stools became more narrow and infrequent.
This was a BIG red flag for me – IBS doesn’t do this, and I wanted to ensure there was nothing suspect going on, so I told him to follow up with his doctor and ensure his colorectal cancer screening was up to date.
Just because you might have IBS, if you have sudden changes in symptoms or any red-flag symptoms – it’s SO important to see your doctor instead of ‘toughing through it’ or assuming it’s just IBS.
Is nausea a symptom of IBS?
I get asked this question frequently. While nausea isn’t a part of the diagnostic criteria for IBS (pain associated with changes in stool frequency and consistency is), nausea is a frequent digestive complaint of those with IBS.
Nausea isn’t traditionally reported in the literature as a symptom of IBS, however, it’s one my patients experience often. In fact, in one study characterizing IBS symptoms, about 25-40% of patients with IBS struggle with nausea (especially those with IBS-M – fluctuating between constipation and diarrhea).
Why? We don’t know the exact answer, however it is likely related to something called ‘visceral hypersensitivity’ (viscera = gut, hypersensitivity = extra sensitive to digestion). 🙁
What is the gut brain axis in IBS?
While your digestion doesn’t necessarily change with IBS, how you sense digestion does, by way of your gut-brain axis. This is the two way information highway between your brain and your gut, that receives information on digestion and mistakenly tells your brain to interpret digestion as pain, discomfort or nausea.
Want to learn more about how the gut-brain axis impacts digestion? Stay tuned for my next research brief on a hot new study looking at brain activity and digestion! 🧠🧠🧠
DOI: 10.1111/nmo.12220

Recent Comments